Cardiomyopathy Homeopathy Treatment in Chennai
- Dr Sheela Homeopathy Clinic Chennai
- Jun 5, 2025
- 6 min read
#cardiomyopathyhomeopathy #cardiomyopathyhomeopathyclinic #cardiomyopathyhomeopathytreatment #cardiomyopathyhomeopathydoctorinchennai #cardiomyopathyhomeopathicclinicinchennai #cardiomyopathyhomeopathictreatmentinchennai #cardiomyopathyhomeopathytreatmentintambaram
Cardiomyopathy Homeopathy Doctor in Chennai
Cardiomyopathy is a term used to describe a group of diseases that affect the heart muscle, impairing its ability to pump blood efficiently to the rest of the body. Unlike many other heart conditions that are caused by blockages in the arteries or valve issues, cardiomyopathy primarily involves structural or functional abnormalities of the myocardium (heart muscle) itself.
This condition can affect people of all ages and may be inherited or acquired due to other medical conditions, lifestyle factors, or unknown causes. Over time, cardiomyopathy can lead to heart failure, arrhythmias, and other serious complications, some of which may be life-threatening. The symptoms can range from mild to severe, and in some cases, individuals may not experience any noticeable signs until the disease has significantly progressed.
Cardiomyopathy is a medical condition that affects the heart muscle (myocardium), reducing its ability to pump blood effectively. Over time, it can lead to heart failure, life-threatening arrhythmias, and other complications. While some forms of cardiomyopathy are inherited, others develop due to lifestyle factors, medical conditions, or unknown causes.
What Is Cardiomyopathy?
Cardiomyopathy is a general term for diseases of the heart muscle that make it enlarged, thick, or rigid. In rare cases, scar tissue replaces the heart muscle. As the disease progresses, the heart becomes weaker and less effective at pumping blood and maintaining a normal electrical rhythm. This can lead to heart failure or sudden cardiac arrest (SCA).

Pathophysiology (How Cardiomyopathy Affects the Heart)
Cardiomyopathy leads to structural and functional changes in the heart muscle:
Systolic dysfunction: The heart muscle loses its ability to contract normally.
Diastolic dysfunction: The heart muscle becomes stiff and doesn’t relax properly.
Electrical instability: Changes in the heart muscle can disrupt the normal electrical signals, leading to arrhythmias.
These changes can result in:
Reduced cardiac output
Ventricular remodeling
Mitral or tricuspid valve regurgitation
Blood clots within the heart
Heart failure symptoms
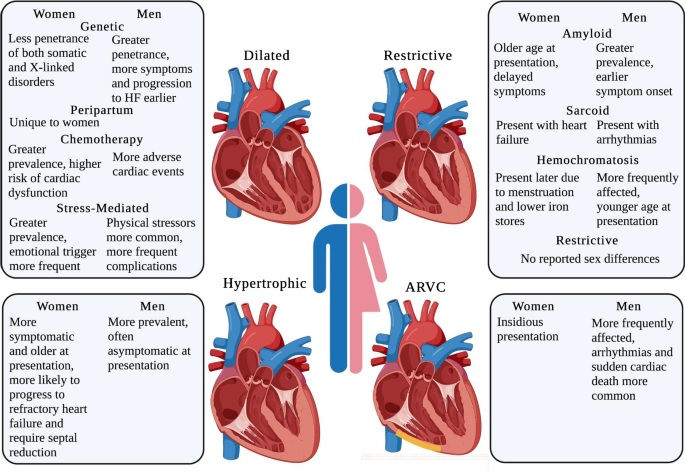
Types of Cardiomyopathy
1. Dilated Cardiomyopathy (DCM)
Description: The left ventricle becomes enlarged and weakened, impairing its pumping ability. In DCM, the heart muscle becomes weakened, and the chambers of the heart (especially the left ventricle) dilate (expand). As a result, the heart's pumping efficiency declines. The heart has to work harder to circulate blood, leading to symptoms of heart failure. Over time, this can lead to arrhythmias (irregular heart rhythms) and even sudden cardiac death.
Causes: Idiopathic (unknown), viral infections, alcohol abuse, certain chemotherapy drugs, genetic mutations.
Common in: Adults aged 20 to 60.
2. Hypertrophic Cardiomyopathy (HCM)
Description: The heart muscle thickens abnormally, especially the interventricular septum. HCM is characterized by the abnormal thickening of the heart muscle, particularly the interventricular septum (the wall between the left and right ventricles). This thickening can lead to a narrowing of the outflow tract of the left ventricle, obstructing the flow of blood. The heart also becomes less able to relax and fill with blood properly, leading to a reduction in its efficiency.
Cause: Usually inherited (genetic mutations in sarcomere proteins).
Risk: Can cause sudden cardiac death, especially in young athletes.
3. Restrictive Cardiomyopathy (RCM)
Description: The heart muscle becomes stiff and less elastic, hindering its ability to fill with blood. In restrictive cardiomyopathy, the walls of the heart become stiff, and the heart loses its ability to expand and fill with blood properly. This reduces the heart's ability to pump blood, leading to heart failure. The condition doesn't usually involve significant thickening of the muscle, but rather fibrosis (scarring) or deposition of abnormal substances in the heart.
Causes: Amyloidosis, hemochromatosis, sarcoidosis, radiation exposure.
Rarity: Least common form.
4. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
Description: Fat and fibrous tissue replace heart muscle in the right ventricle, disrupting electrical signals. In ARVC, the heart muscle in the right ventricle is replaced by fatty or fibrous tissue, leading to impaired contraction of the right ventricle. This can cause arrhythmias, particularly ventricular arrhythmias, which are irregular heartbeats originating in the lower chambers of the heart.
Cause: Genetic (desmosomal protein mutations).
Common in: Young adults; may cause sudden death in athletes.
5. Takotsubo Cardiomyopathy (Stress Cardiomyopathy)
Description: A temporary condition mimicking a heart attack, often triggered by emotional or physical stress. Takotsubo is a temporary condition where the left ventricle of the heart becomes abnormally enlarged and weakened, usually after intense emotional or physical stress. The exact mechanism is not fully understood, but it is believed that stress hormones (like adrenaline) may cause spasm of the coronary arteries or direct damage to the heart muscle.
Cause: Sudden surge of stress hormones.
Outcome: Usually reversible with proper care.
6. Peripartum Cardiomyopathy
Description: A rare form of cardiomyopathy that occurs during the last month of pregnancy or within five months after delivery. The heart's ability to pump blood is reduced.
Causes: The exact cause is unknown but may involve hormonal changes, high blood pressure, or inflammation.
7. Ischemic Cardiomyopathy
Description: Occurs when the heart muscle is damaged due to a lack of blood supply, typically caused by coronary artery disease or a previous heart attack. The heart becomes weakened and dilated.
Causes: A history of coronary artery disease or heart attack.

Causes of Cardiomyopathy
Genetic mutations (especially in HCM and ARVC)
Infections (e.g., viral myocarditis)
Chronic high blood pressure
Heart valve diseases
Metabolic disorders (e.g., diabetes, thyroid disease)
Nutritional deficiencies (e.g., thiamine or selenium)
Alcoholism or drug abuse
Toxins and chemotherapy
Autoimmune diseases
Pregnancy-related cardiomyopathy (peripartum cardiomyopathy)
Symptoms of Cardiomyopathy
Symptoms may be absent early on but typically worsen as the disease progresses:
1. Shortness of Breath (Dyspnea)
At rest or during physical activity
May worsen when lying flat (orthopnea)
May wake a person from sleep (paroxysmal nocturnal dyspnea)
2. Fatigue and Weakness
Due to poor blood flow and oxygen delivery to tissues
3. Swelling (Edema)
In the legs, ankles, feet, or abdomen (ascites)
Caused by fluid buildup due to poor circulation
4. Chest Pain or Discomfort
Often brought on by exertion or stress
Can mimic angina or heart attack symptoms
5. Palpitations
Sensation of a racing, fluttering, or pounding heart
Caused by arrhythmias (irregular heartbeats)
6. Dizziness or Lightheadedness
May occur with or without exertion
Can lead to fainting (syncope), especially in hypertrophic or arrhythmogenic types
7. Cough
Persistent, especially when lying down
Often due to fluid buildup in the lungs (congestive heart failure)
8. Decreased Exercise Tolerance
Getting tired quickly or feeling winded even during mild activity
9. Sudden Cardiac Arrest
Rare but possible, especially in hypertrophic or arrhythmogenic types
Complications
Without appropriate treatment, cardiomyopathy can lead to serious complications:
Heart failure
Arrhythmias (e.g., atrial fibrillation, ventricular tachycardia)
Stroke (due to blood clots forming in the heart)
Cardiac arrest
Valve problems (especially mitral or tricuspid regurgitation)
Sudden cardiac death
Risk Factors
You may be at increased risk for cardiomyopathy if you:
Have a family history of cardiomyopathy, heart failure, or sudden cardiac death
Have hypertension, diabetes, or obesity
Abuse alcohol or recreational drugs
Have had chemotherapy or radiation to the chest
Have certain infections or autoimmune disorders
Are a competitive athlete with undiagnosed HCM or ARVC
Are pregnant or have had recent childbirth (peripartum cardiomyopathy)
Cardiomyopathy Homeopathy Treatment in Chennai
Frequently Asked Questions
1. What are the risks of sudden cardiac arrest with cardiomyopathy?
Answer: Sudden cardiac arrest is a significant risk in hypertrophic cardiomyopathy (HCM), arrhythmogenic right ventricular cardiomyopathy (ARVC), and dilated cardiomyopathy (DCM) in some cases. Implantable cardioverter defibrillators (ICDs) can help prevent this by detecting and correcting life-threatening arrhythmias.
2. How does peripartum cardiomyopathy differ from other forms of cardiomyopathy?
Answer: Peripartum cardiomyopathy occurs during the last month of pregnancy or within five months after childbirth. It can lead to heart failure, and its exact cause is unclear, although hormonal and immune factors are believed to play a role.
3. Can stress cause cardiomyopathy?
Answer: Yes, Takotsubo cardiomyopathy, also known as stress-induced cardiomyopathy or broken heart syndrome, is often triggered by extreme emotional stress like the death of a loved one, trauma, or sudden shock. This type of cardiomyopathy is usually temporary and often resolves on its own.
4. Is it safe to exercise with cardiomyopathy?
Answer: Exercise is often recommended, but it must be tailored to the individual and should be done under a healthcare provider’s supervision. Hypertrophic cardiomyopathy (HCM) patients, in particular, may need to avoid intense physical exertion due to the risk of arrhythmias.
5. Can cardiomyopathy cause heart failure?
Answer: Yes, cardiomyopathy can lead to heart failure, where the heart cannot pump enough blood to meet the body's needs. This is especially common in dilated cardiomyopathy and restrictive cardiomyopathy.


